
It’s my belief that we can help our patients manage chronic breathlessness better.
Chronic breathlessness management is an all too often neglected part of healthcare professional training, and it can be a challenging symptom to support your patient in managing better. Chronic breathlessness is one of the most common reasons patients may present to primary or emergency care.[1],[2]
This article will give you some important hints and tips on how to support your patients better such as:
- understanding the emotions and behaviours that can influence chronic breathlessness,
- teaching your patients some breathing techniques to manage their breathlessness better, and
- other services you can refer patients on to for additional support.
Breathlessness is a subjective, distressing sensation of awareness of difficulty with breathing which can be acute, subacute or chronic, with chronic breathlessness developing slowly over weeks or months.[3]
Chronic breathlessness can be caused by a large range of conditions such as asthma, COPD, heart failure, deconditioning, obesity, neurological problems, anaemia, and breathing pattern disorders.[3] Over two-thirds of chronic breathlessness is caused by cardiorespiratory disease.[3]
The first step in managing chronic breathlessness is to identify and treat the underlying cause – this may sound simple, but it can be a challenge especially if your patient has multiple conditions contributing to the levels of breathlessness they are experiencing.
The next important step is to support your patient with lifestyle changes – e.g. supporting smoking cessation, increasing physical activity, or nutritional advice and support to maintain a healthy weight.[4] Although this sounds easy, it can be challenge in clinical practice, so it’s worthwhile spending time understanding your patient and their potential barriers to lifestyle interventions.
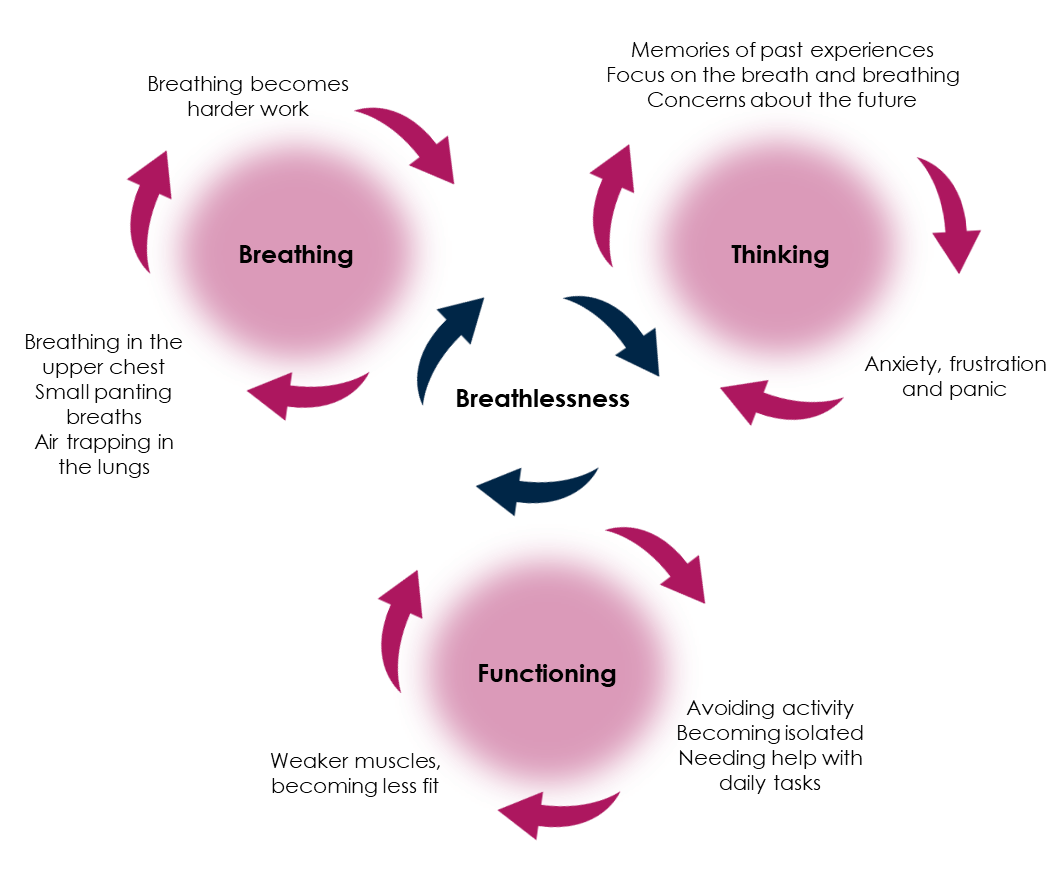
You can also explain chronic breathlessness and the causes to patients using a chronic breathlessness framework such as the Breathing, Thinking, Functional model.[5] This can help to explain the normal emotional and behavioural responses to breathlessness, and shows how these can form vicious cycles that inadvertently worsen their symptom.[5]
The model can explain why breathlessness can seem out of context to the underlying condition, and why breathlessness can persist after a chest infection has settled.[5] Using this framework can help you in selecting appropriate non-pharmacological treatments to support breathlessness management.[5]
Breathlessness management
Some non-pharmacological treatments that can help to reduce breathlessness management can be used with ease in the primary care setting. These include:
Fan therapy
A small handheld fan, held a few inches from the face and moved slowly side to side can help to reduce the sensation of breathlessness.[6]
Teaching relaxed breathing (diaphragmatic breathing)
This involves breathing using the diaphragm, rather than accessory muscle in the neck and top part of the chest. Breathing using the diaphragm is more efficient and uses less energy, reducing the sensation of breathlessness.[7]
To practice diaphragmatic breathing, your patient would use the following steps:[7]
1. Sit somewhere quiet where you won’t be disturbed, and your arms are well supported
2. Place one hand on the top of your chest and the other hand on the top part of your stomach. To begin with, feel where the movement is coming from
3. Try to breathe in slowly through your nose (if able) and out through your mouth. Think about keeping your shoulder and arms as relaxed as you can
4. As you breath in your stomach should rise and the top part of your chest should stay still. Your stomach should fall as you breath out
5. Slow your breathing down as you feel comfortable to, you breath out should be longer than your breath in.
Patients need to regularly practice this way of breathing several times a day and gradually increase the duration to help manage episodes of breathlessness effectively.[7] Once your patient can use breathing control, you can add in other breathing techniques to manage breathlessness.
Rectangle breathing
This breathing technique is helpful to slow your breathing rate down and can be used to help recover from exertion. To practice rectangle breathing, your patient would use the following steps:[8]
1. Find something rectangle shaped to look at (such as your TV, mirror or picture) and sit yourself comfortably in front of it
2. Follow the outline of the shape with your eyes whilst doing the relax breathing described above
3. Breathe in whilst following the short sides of the rectangle and breathe out following the longer sides.
Pursed lip breathing
This type of breathing is helpful to control breathlessness when doing something that requires more effort. To practice pursed lip breathing, your patient would use the following steps:[8]
1. Breathe in through your nose (if you can)
2. Purse your lips together as if you are going to blow out a candle or whistle
3. Gently breathe out through your pursed lips for as long as is comfortable
4. Don’t force the air out of your lungs.
Paced breathing
This can be combined with pursed lip breathing to use during activity to prevent breath holding, which makes breathlessness worse. It can be helpful for climbing stairs and walking. To practice paced breathing, your patient would use the following steps:[9]
1. Count whilst you are breathing – so count to one as you climb one step (breathing in while you count)
2. Then count for two as you climb the next two step (breathing out whilst you count)
Panic and breathlessness
If your patients report they get panicky and breathless, they can try recovery breathing and the three F’s – for COPD and asthma that means:[8]
• fan
• forward lean
• focus on long breaths out.
For other conditions the three F’s mean:
• fan
• flop (drop your shoulders)
• focus on relaxed breaths out.
Helping patients with planning and pacing of activity during the day can support managing breathlessness, by not rushing or overdoing activity.[9]
A multidisciplinary approach
Involving the wider multidisciplinary team in the management of chronic breathlessness is important. Referrals to the following services and teams may be considered appropriate for your patients:[3]
• pulmonary rehabilitation for people with chronic respiratory disease that get breathless daily. This team can also support with more detailed breathlessness management and chest clearance techniques
• occupational therapy services can support with home adaptations to help patients maintain independence at home
• community physiotherapy services can offer mobility aids to reduce breathlessness whist walking and exercise programmes if pulmonary rehabilitation is not suitable
• equipment services to help maintain independence and reduce breathlessness during activities in and out of the home, including wheelchair services as required
• dieticians can support with nutrition, especially if breathlessness whilst eating is a problem
• speech and language therapy can support with communication and problems with swallowing
• social services if care needs are identified
• local exercise referral schemes to support patients to be more physically active
• psychological support.
Useful resources
Here are some useful resources for yourselves, your colleagues, and your patients:
- Physiotherapy for Breathing Pattern Disorders
- NHS England eLearning portal
- Association of Chartered Physiotherapists in Respiratory Care – Patient Information
- Asthma + Lung UK – Living well with breathlessness
- Primary Care Respiratory Society – Top tips for communicating the benefits of pulmonary rehabilitation to patients
- Primary Care Respiratory Society – Top tips for encouraging activity as a gateway to good respiratory health
Conclusion
There is always something we can do to help patients experiencing breathlessness:
- treat and optimise management of the underlying condition(s) contributing to the breathlessness
- refer to other services that can support, such as pulmonary rehabilitation, occupational therapy, community rehabilitation, and equipment services
- signpost your patients to support groups and online resources.
Most importantly – teach your patient techniques to manage their breathlessness, such as breathing control, fan therapy and box breathing. If these don’t work, always refer on or seek help from others. Supporting your patients to manage their breathlessness is an achievable aim.
Any advice given and opinions expressed in this article are those of the author and do not reflect the view of Chiesi Limited (Chiesi). All content in this article is for informational and educational purposes only. Although Chiesi strives to always provide accurate information, it is not responsible for and does not verify for accuracy any of the information contained within.
[1] Frese T, Sobeck C, Herrmann K et al. J Clin Med Res. 2011; 3(5): 239-46
[2] A Pickering, A Williams, JM Bland et al. BMC Plum Med. 2017: 53 (1)
[3] NHS England. Adult breathlessness pathway (pre-diagnosis): diagnostic pathway support tool. Available at: www.england.nhs.uk/long-read/adult-breathlessness-pathway-pre-diagnosis-diagnostic-pathway-support-tool/
[4] Asthma + Lung UK. Living well with breathlessness. Available at: www.asthmaandlung.org.uk/symptoms-tests-treatments/symptoms/breathlessness/breathlessness/living-well-breathlessness
[5] University of Cambridge. Breathing, Thinking, Functioning. Available at: www.btf.phpc.cam.ac.uk/what-is-the-btf-model/
[6] Qian, Yu et al. Journal of Pain and Symptom Management. 2019: 58(3): 481 – 486
[7] Cleaveland Clinic. Diaphragmatic Breathing. Available at: https://my.clevelandclinic.org/health/articles/9445-diaphragmatic-breathing
[8] Cambridge University Hospitals. Breathing techniques to ease breathlessness. Available at: www.cuh.nhs.uk/patient-information/breathing-techniques-to-ease-breathlessness/
[9] Supporting breathlessness. Pacing. Available at: www.supporting-breathlessness.org.uk/support_copd/living-a-fulfilling-life/pacing/



 Sam Hayes
Sam Hayes 

