
Improving outcomes for people with COPD is central to optimal disease management. To achieve this requires a holistic impact assessment to reduce symptoms of the disease, and to reduce the risk of adverse events.[1]
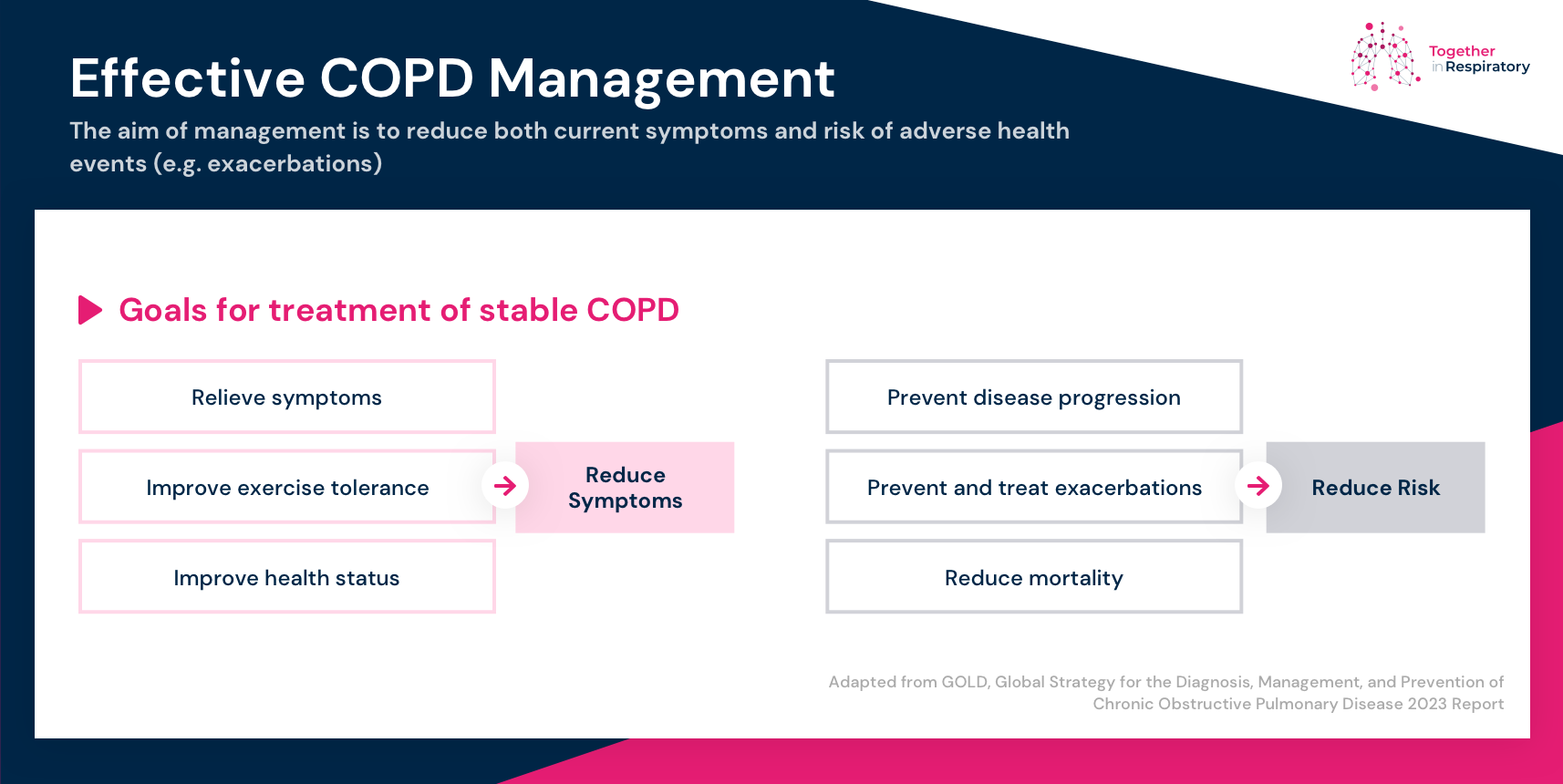
Both the Global Initiative for Chronic Obstructive Lung Disease GOLD report[1] and the NICE guidelines[2] recommend a comprehensive assessment of the impact of COPD on the individual, to plan treatment and management accordingly. This includes assessment of:[2]
- the degree of airflow limitation
- breathlessness and impact on activity
- severity and frequency exacerbations
- multimorbidity and frailty.
Let’s look at each of these in turn.
Airflow limitation
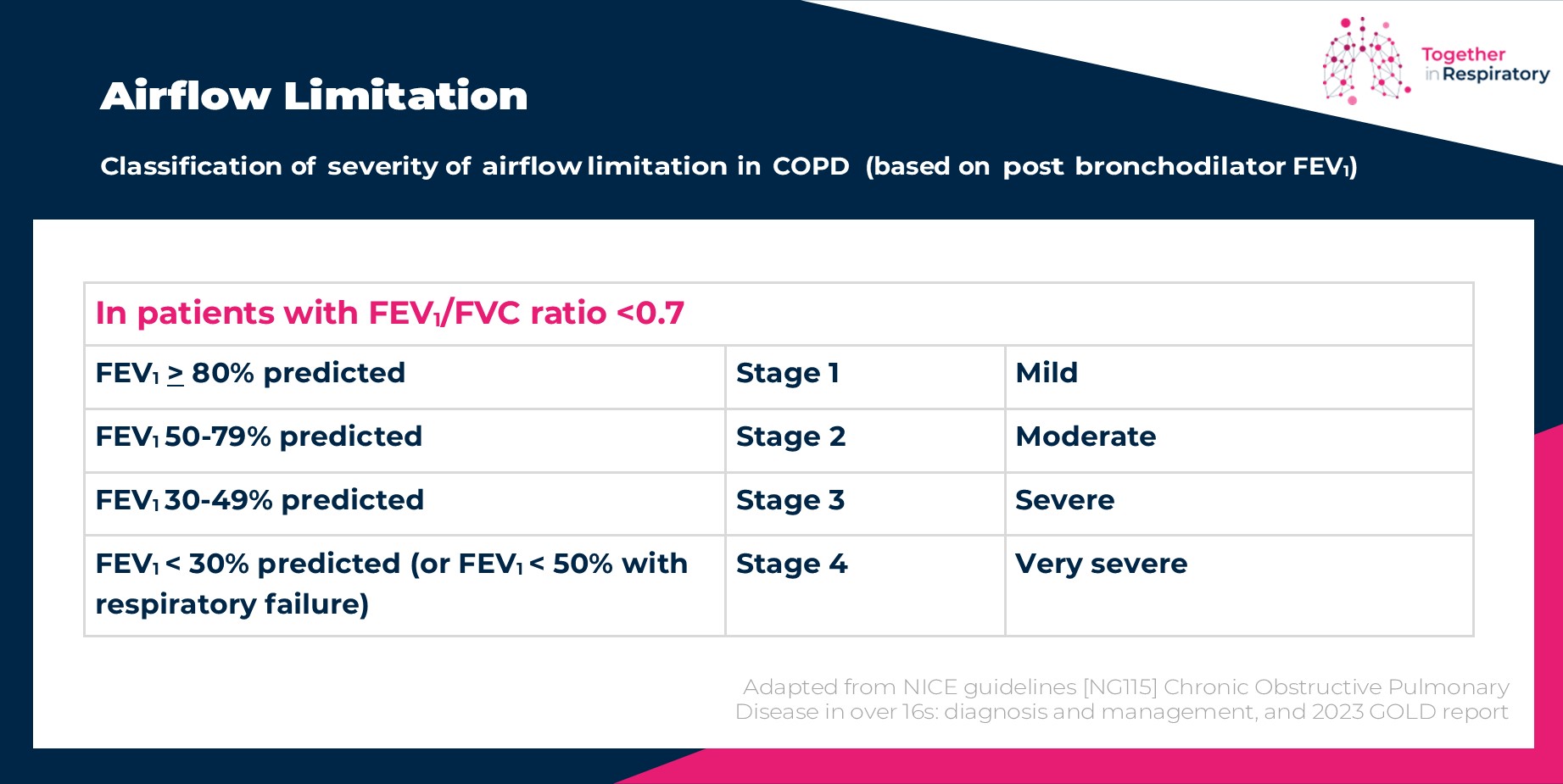
The National Institute for Health and Care Excellence (NICE) guidelines and Global Strategy for Prevention, Diagnosis and Management of COPD (GOLD) report for COPD support the diagnosis of airflow limitation when FEV1/FVC ratio is <0.70.[1],[2] The fixed ratio <0.70 was chosen to separate normal from abnormal since it identified a population in which airflow limitation was associated with disease.[3]
Note: Using a fixed value of <0.70 may underestimate airflow limitation in younger individuals and may overestimate airflow limitation in older people.[1] Guidelines therefore also suggest using the lower limit of normal (LLN), representing the lower 5% of test results from a normal population, as this may improve accuracy of diagnosis in these groups.[1]
Once the presence of airflow limitation is confirmed, the severity of airflow limitation is classified using post bronchodilator FEV1 % predicted.[1],[2]
Assessing breathlessness and impact on activity
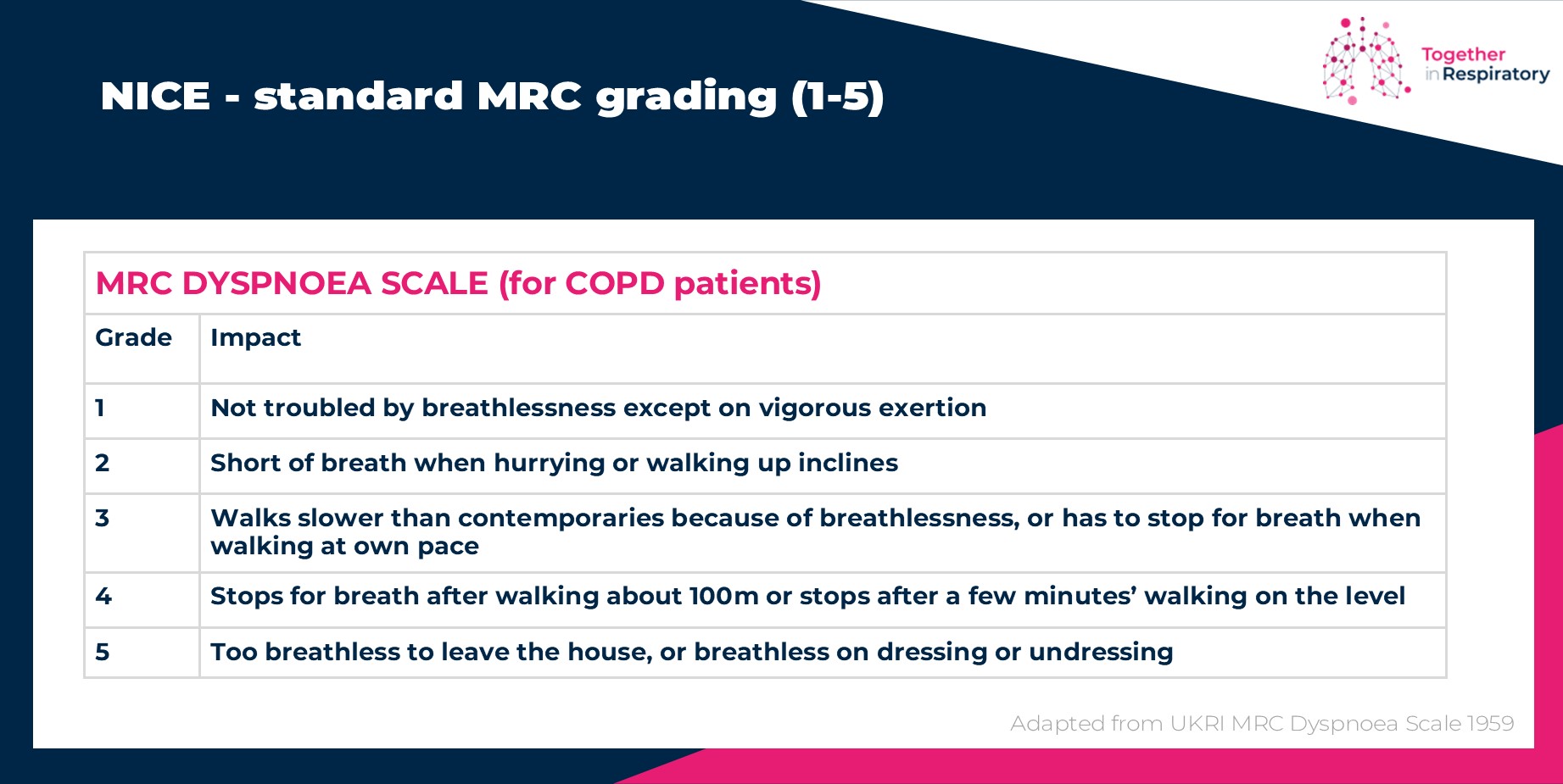
One of the primary symptoms of COPD is breathlessness.[2] Guidelines recommend that the Medical Research Council (MRC) dyspnoea scale should be used to grade breathlessness according to the level of exertion required to elicit it.[2]
MRC Dyspnoea Scale
This scale has been in use for many years for grading the effect of breathlessness on daily activities. [4] The scale measures perceived respiratory disability, using the World Health Organization (WHO) definition of disability being “any restriction or lack of ability to perform an activity in the manner or within the range considered normal for a human being”.[4]
The MRC Dyspnoea Scale is simple to administer as it allows the patients to indicate the extent to which their breathlessness affects their mobility.
Confusingly, NICE use the standard MRC grading (1-5),[2] whereas the GOLD report uses the mMRC (Modified Medical Research Council) Dyspnoea Scale.[1] which is very similar to the original but is graded 0-4. In practice it is important to be clear which scale is being used at the time of assessment so that accurate comparisons can be made over time.
Importantly, MRC score of 3 or more (mMRC 2) is frequently used to identify people with COPD who should be referred for pulmonary rehabilitation.[2] Check the referral criteria for your local service.
COPD Assessment Test
The COPD Assessment Test (CAT) was developed as a short, simple questionnaire to provide a framework for discussions with COPD patients and their healthcare professionals to enable a common understanding and grading of the impact of the disease on the patients’ lives.[5]
The CAT is not a diagnostic tool,[6] but it can help monitor the effects of treatment and management. In practice, I find the CAT is quick and easy for patients to complete and succinctly helps identify where COPD has the greatest impact on the patient’s health and daily life. It supports clinicians to be better informed when discussing and making management decisions with patients and to ensure that their health status is as good as it can be.
Exacerbations
Exacerbations of COPD are important events that can negatively impact health status, rates of hospitalisation, and disease progression.[1] Factors that increase the risk of exacerbations include a history of exacerbations and raised blood eosinophils.[7]
The GOLD report defines an exacerbation as:[1]
“…an event characterized by dyspnoea and/or cough and sputum that worsen over <14 days, which may be accompanied by tachypnea and/or tachycardia and is often associated with increased local and systemic inflammation caused by airway infection, pollution, or other insult to the airways.”
NICE 2019, suggest the following classification to grade the severity of exacerbations as:[2]
- mild exacerbation, the person has an increased need for medication, which they can manage in their own normal environment
- moderate exacerbation, the person has a sustained worsening of respiratory status that requires treatment with systemic corticosteroids and/or antibiotics
- severe exacerbation, the person experiences a rapid deterioration in respiratory status that requires hospitalisation.
Multimorbidity and frailty
Most patients with COPD suffer multimorbidity linked to shared risk factors including smoking, aging, and inactivity, which may have a major impact on health status and survival.[1]
Airflow obstruction and particularly hyperinflation affect cardiac function. The overspill of inflammatory mediators from the lung into the circulation may also contribute to skeletal muscle wasting and initiate or worsen comorbidities such as ischemic heart disease, heart failure, osteoporosis, normocytic anaemia, diabetes, and metabolic syndrome.[1]
Further, the prevalence of depression and anxiety in individuals with COPD is high and the prevalence of panic disorder is approximately ten times higher in people with COPD than in the general population.[8]
Mental health issues in COPD are associated with reduced ability to cope with physical aspects of the illness, a poorer quality of life, more frequent hospital admissions with longer length of stay, reduced medication compliance and lower adherence to rehabilitation and other treatment regimes.[8]
Screening for comorbid disease and careful assessment of the interplay between multimorbidity, mental health issues and COPD is therefore needed.
Any advice given and opinions expressed in this article are those of the author and do not reflect the view of Chiesi Limited (Chiesi). All content in this article is for informational and educational purposes only. Although Chiesi strives to always provide accurate information, it is not responsible for and does not verify for accuracy any of the information contained within.
[1] Global Initiative for Chronic Obstructive Lung Disease. 2023 GOLD report. Available at: https://goldcopd.org/2023-gold-report-2/
[2] NICE. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Available at: https://www.nice.org.uk/guidance/ng115/chapter/Recommendations
[3] Smith, LJ. The lower limit of normal versus a fixed ratio to assess airflow limitation: will the debate ever end? Eur Respir J. 2018; 51: 1800403
[4] UK Research and Innovation. MRC Dyspnoea Scale. Available at: https://www.ukri.org/councils/mrc/facilities-and-resources/find-an-mrc-facility-or-resource/mrc-dyspnoea-scale/
[5] The COPD Assessment Test (CAT). Clinical Practice. Available at: https://www.catestonline.org/hcp-homepage/clinical-practice.html
[6] Ghobadi, H. et al. The Relationship between COPD Assessment Test (CAT) Scores and Severity of Airflow Obstruction in Stable COPD Patients. Tanaffos. 2012; 11(2): 22-26
[7] Hurst J, Skolnik N, Hansen G et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Euro. J. of Int. Med. 2020; 73: 1-6
[8] Wang J, Willis K, Barson E. et al. The complexity of mental health care for people with COPD: a qualitative study of clinicians’ perspectives. npj Prim. Care Respir. Med 2021; 31(40)



 June Roberts
June Roberts 

